بیمار نیکان عضوی از خانواده ماست
Glaucoma
What is Glaucoma?
The possibility of chronic diseases is directly related with aging. Accordingly, doctors suggest that middle-aged people undergo annual medical checkups. Glaucoma is an eye disease appearing mostly in people over 50 years old. Up to 2% of people suffer from glaucoma. Unfortunately, many of the patients are not aware of their disease.
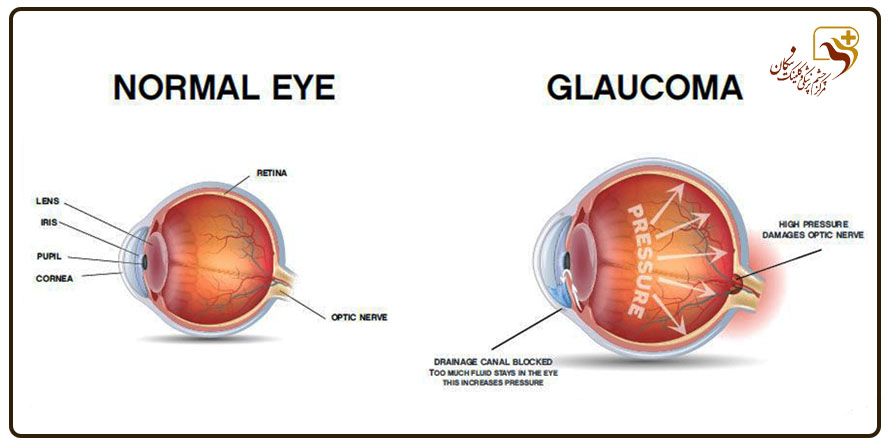
Glaucoma means increased intraocular pressure that can damage the optic nerve and result in irreversible vision loss. It should be known that some types of glaucoma can have no symptoms until the final stages of the disease, and when a person realizes his disease, many fibers of his optic nerve have been destroyed and his vision has severely and irreversibly decreased. Therefore, early diagnosis of glaucoma and starting treatment on time will be the main key in preventing the progression of the disease and reducing the patient’s vision.
A clear liquid is constantly secreted in the eye, which is called aqueous humor, and this liquid comes from a place called the angle (where the cornea meets the iris). If for some reason, there is a blockage or an obstacle in the way of exiting this liquid in the eye and the aqueous humor cannot easily leave the eye, the pressure inside the eye increases.
Types of glaucoma
- Acute closed angle glaucoma;
- Chronic or primary open-angle glaucoma;
- Low-pressure or normal pressure Glaucoma;
- Congenital glaucoma;
- Inflammatory glaucoma;
- Neovascular (vascular) glaucoma;
- Secondary glaucoma and the use of steroid drugs.
What are the symptoms of glaucoma?
In most patients, there are few signs and symptoms. But in the advanced stages, the following symptoms are seen:
Who are the people prone to glaucoma?
- Those old above 40 years;
- Glaucoma family history;
- Myopia;
- Lack of thickness of the cornea;
- Blacks;
- hyperopia;
- Diabetes;
- Cardiovascular disease.
People at risk should undergo an eye examination according to a specific schedule.
Post-operative referrals
Always, the first visit after the operation should be the first day after the surgery, doctor must be consulted about the next visits. Do not forget to always bring your medicines with you in the next visits.
Eye protection
In the first week after the operation, use an eye protection cover (perforated shield), especially when sleeping. To avoid eye damage and strong light, you can use sunglasses during the day, especially outdoors.
Daily activities
You can resume daily activities including walking and watching TV a few days after the operation. Of course, intense physical activities such as lifting heavy objects, swimming, aerobics, and impact sports, etc. should be avoided for one to two months.
In glaucoma surgery, pray sitting and do not bow your head down for prostration up to one to two weeks after the operation.
Face wash
In the first 3 to 5 days after the operation, avoid splashing water on the face and eyes. Use a clean and wet towel to wipe your face.
Taking a bath
There is no problem in washing the body (from the neck down) after the first day; however, do not take a shower or bath in the tub for 72 hours after the operation. Of course, it is recommended to consult your doctor before taking a bath. You can bend your head back to wash your hair so that water drops don’t fall into your eyes.
Use of cosmetics
Eye make-up should be avoided for four to six weeks. It may be better to avoid eye make-up while using post-operative drops.
Diet
Diet is not subject to any restriction and usual diet can be kept. Of course, pre-existing diets for underlying diseases (including diabetes and high blood pressure) should be followed. To prevent constipation, consume a diet containing fiber and liquids.
Driving
Never drive without an ophthalmologist’s permission, especially at nights. Make sure to consult your doctor about the need to use glasses (sunglasses or medical glasses) for driving.
Natural symptoms
The following symptoms are normal after glaucoma surgery and are not alarming:
Slight redness, slight epiphora, blurred vision, foreign object sensation and slight ptosis; The symptoms should disappear gradually within four to six weeks after the operation.
Warning signs
In cases of increasing pain, severe sensitivity to light, epiphora, eyelid and conjunctival swelling, reduced vision in the operated eye, and in case of nausea and vomiting, you should contact your doctor immediately.
Drops used after glaucoma surgery
Usually, three types of drops are prescribed for the patient after the glaucoma operation:
- Cortone or steroid drops such as betamethasone, dexamethasone, fluorometholone or prednisolone
- Antibiotic drops such as chloramphenicol, sulphastamide or ciprofloxacin
Normally, the drops and medicines used before glaucoma operation are stopped, but the doctor must be consulted in this regard. At the same time, the use of the above drops is only related to the operated eye and it should be avoided to pour it in the opposite eye. Moreover, if you use anti-glaucoma drops in the opposite eye (non-operated eye), never stop using it in the non-operated eye. Normally, during the night (12 pm to 6 am) there is no need to pour drops.
Other drugs
Your doctor may prescribe acetazolamide (Diamox) to control eye pressure after surgery. Be sure to consult your doctor about the amount and duration of use.
You can keep taking other preoperative medications (such as those for diabetes and blood pressure control) after glaucoma surgery. Consult your doctor about taking aspirin and anticoagulants.
If you feel mild pain, you can use one acetaminophen tablet every four to six hours, but in the case of severe and increasing pain accompanied by decreased vision, you must consult your doctor.
It is very important to observe the following regarding post-operative medications:
- Take the medicine exactly as prescribed by the doctor.
- Do not forget the times when the ointment or drops should be used.
- If you use ointment and drops in the same eye, always put the drop in the eye first and use the ointment after five minutes.
- In the summer season, you can keep the ointment and drops in the refrigerator between uses.
- Do not let others use your drops or ointments.
- Discard drops and ointment after four weeks of first use.
- Keep drops and ointment out of the reach of children.
- Bring your eye medications with you every visit.